Barriers and Solutions to Comprehensive Care for Mental Health Patients in Hospital Emergency Departments
Elizabeth Levin1*, Husam Aburub2
1Department of Psychology, Laurentian University, Sudbury, Ontario, Canada
2Health Sciences North, Sudbury, Ontario, Canada
Abstract
Hospital emergency departments in Ontario, have become a common place for patients with mental health problems to seek treatment. Studies report healthcare providers have limited knowledge and competency to provide optimal care for patients with mental health problems. As a result, these patients are at risk of poor hospital experiences and treatment outcomes. In addition, emergency staff report considering patients with mental health problems lower priority to other patients. This paper reviews the existing literature and examines the challenges surrounding patients with mental health problems seeking treatment in emergency rooms and how it leads to sub-optimal care. Strategies are then shared to overcome these challenges by changing emergency department experiences for mental health patients seeking treatment.
Emergency Departments - a Resource for Mental Health Services
Mental health problems affect one in four people, who often visit emergency departments as the first point of contact with the healthcare system, and as a last resort for mental health services.1 Clarke, et al., estimate that between 5 and 10% of emergency department patients in Canada are individuals with mental health issues.2 Zun and Downey estimate that 45% of adults who present to the emergency department with physical complaints have undetected mental health issue.3 As a result, the number of patients who visit the department with mental health concerns may be higher than reported. Khan et al., report that between 2006-2011, in Canada, emergency department visits for mental health services rose by 33%.4 The Canadian Institute for Health Information reports that between 2006 and 2016, there was a 50% increase in emergency department visits by youth with mental disorders.5 Most importantly, this growth occurred despite warnings that emergency departments are not ideal for these patients.1,6
This paper provides a narrative review of the literature on the use of emergency departments by mental health patients and offers recommendations to improve the experience for both patients, staff and the community. The review was conducted using search terms such as mental health patients, emergency departments, mental health care, and hospital care for mental health patients looking for relevant research from 2010 onwards using Medline and PsycInfo.
Barriers to Comprehensive Care of Mental Health Patients in the Emergency Department
Emergency departments are accessible 24 hours a day and focus on providing care for patients with physical problems. The challenge to optimal care for mental health patients initially occurs during triage. Emergency department nurses admit to a lack of expertise and confidence when triaging mental health patients.7 As a result, mental health patients have longer wait times as they are deemed less urgent.2
Many emergency departments have an open environment, which can be ineffective when dealing with mental health patients where privacy and confidentiality are paramount. The emergency department waiting area is an overwhelming, overstimulating area.8,9 Patients often have limited access to food, drink, toilets, privacy and telephones and some are waiting against their will. These factors, in combination with perceived long wait times culminate in feelings of agitation, restlessness, emotional distress and overall dissatisfaction in these patients and their families.1,2 As a result, the stay in emergency may not improve their condition.6,10
Worldwide, emergency departments face significant challenges in delivering comprehensive care because of increasing patient numbers and limited resources.11 Some common barriers to effective mental healthcare in emergency departments include: a reduction in psychiatric beds; lack of resources, especially during busy hours; a long and slow diagnostic process; safety concerns; suboptimal training of emergency department staff; and poor follow-up strategies.
Figure 1 presents the six barriers to comprehensive care in its outer layer, with the results of each individual barrier shown beside each larger rectangle.
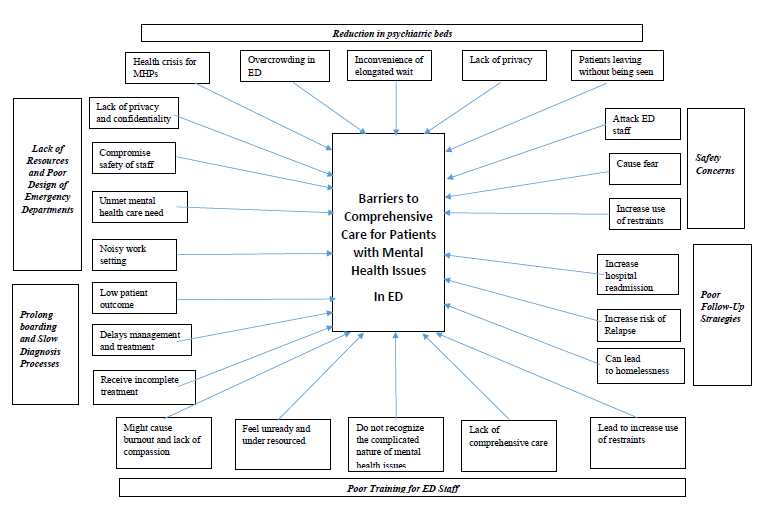
Figure 1: Barriers Affecting Mental HealthCare in the emergency department.
Solutions to Barriers
An Increase in Inpatient Settings and Community Mental Health Services is Required
Deinstitutionalization was designed to improve the treatment of mental health patients and reduce government spending.12 The development of psychiatric medications contributed to thousands of mental health patients being released between 1960-1990 as psychiatric hospitals closed. These closures reduced or ended long-term, in-patient care services.10,13 Recognizing that people with mental health issues needed to be treated rather than locked away also led to increased use of beds in general hospitals.14-16 Hospitalization for mental health remains a key component of healthcare.17 Insufficient community services leads to increased mental health patients in the emergency department.18 Patients become chronic, and early discharge increases the risk of homelessness, arrest, abuse, and crises thereafter. Well-intentioned deinstitutionalization implementation created lapses, which were transformed into an inefficient and ineffective mental health change policy.19
Nevertheless, some excellent treatment examples exist such as the model of care employed by the City of Trieste, Italy.19 The Trieste Model is deemed by the World Health Organization as one of the most progressive mental health systems globally.20 When 1,200 mental health beds closed, the state addressed the needs of outpatients by developing housing, round-the-clock community centres, home care, social clubs, work cooperatives, and recreational opportunities. The Trieste Model offers elegant environments for these patients, supported by enthusiastic care providers, and a broad spectrum of initiatives aimed at integrating them into the community.20 The primary goal of this model is to supply therapeutic, social, and rehabilitative continuity to users. This is accomplished by creating and sustaining a social atmosphere into which patients, family members, and friends are welcomed to take part in available activities.19 Since the overall goal is to integrate mental health patients into the community, this framework, together with its activities, seeks to make that transition seamless.
The Trieste Model embodies the original idea behind deinstitutionalization. Nevertheless, some evidence suggests that most approaches used in the United States fall short of the ideals of the policy.16 Another solution proposed by Yohanna suggested that hospitals return to their traditional role for mental health including permitting involuntary commitment.21 That study was partially conducted in Canada, meaning similar measures should be effective here.21
Improve Resources and Mental Health Patient Flow in Emergency Departments
Overcrowding results in patients waiting and influences triage, which increases the number of waiting patients and their distress.8,10 The limited staff is often incapable of providing needed care. Patients classified as non-urgent, feel that they are a problem. Even though every patient needs to undergo proper evaluation, the majority of emergency departments struggle to provide mental health services.22
A growing number of Canadian provinces cut services for mental health patients including community, and hospital-based psychiatric care. Overall, this forced many such patients to resort to the emergency department.12,21 However, since these operate on a tight budget, physically ill patients, are easier and more efficient to prioritize.22 Only a few emergency departments have psychiatrists on staff, and most emergency department staff are not trained in psychiatry.11,14 The few patients seen by psychiatrists receive quality, effective care.7
Meanwhile, emergency departments are increasingly seen as the only remaining safety net for mental health patients.23 Since this is where change should start, the need to redesign the physical and operational layouts of these units is imperative. An excellent model of a redesigned emergency department was reported at the Thunder Bay Regional Health Sciences Centre in Ontario.24 This facility, recognized mental health patients need a calm and quiet environment to stabilize. The new serene design has a stabilization unit where mental health patients can be assessed and observed without interference from other emergency department patients or staff.
Another effective resource is telemedicine. Widely used in Canada, especially in mental healthcare,25 telepsychiatry has led to a 30% reduction in time to treatment, length of stay, and door-to-door consult time.26 Telepsychiatry provides safe mental health assessment. A successful model using telepsychiatry is the Burke Center in Lufkin, Texas.27 This facility operates uses remote supervision by telepsychiatrists to deliver on site care by a multidisciplinary team. The model requires patients to be treated and discharged within 24 hours, decreasing hospital admission, leaving more open inpatient beds. There is a need for dedicated staff and exclusive treatment space to integrate this approach into the emergency department.
Rutman et al., advocated for the use of the Lean model to improve healthcare; a systematic method with a focus on follow up and communicating results for sustainability.28,29 The Lean approach leads to improved emergency department wait times and quality of care, savings, and allows hospitals to ascertain areas of their operation that may be redundant or costly.30 Using savings, hospitals invest in areas that need additional funding.31 The Lean process focuses on continuous improvement, elimination of waste, promotion of flow, and leadership development. The process complements patient-centered clinical goals.29
The car company Toyota created a system where the whole production line would stop when a problem was identified, so the problem could be dealt with in a short time. The Lean system isolates these customers/patients, finding out their views of value addition, and puts measures in place to achieve it. Any identified waste that cause patients to wait is eliminated. New processes are introduced to ensure that everything aligns to demands, and leads to continuous improvement. The healthcare sector has realized success using this system in the United States, Australia and Canada.31
Lean implementation improved flow through the emergency department at a West Coast Hospital and the Seattle Children’s Hospital emergency department by reducing length of stay for all patients.10,28 The Lean system works only if implemented as a series of small steps that eventually culminate in overall improvement.10 In the mental health emergency department context, staff should work with patients to identify processes that add value and strive to align treatment expectations. The goals are to achieve positive change, better quality healthcare, and employee involvement.31 The tendency to categorize mental health patients into one group should also cease so that each patient is treated on a case-by-case basis. For mental health patients, this adjustment requires the emergency department to establish working relationships with outpatient facilities where patients can be directed.31 Staff create ‘care paths’ to standardize operations and more easily provide the proper treatment.10
A ‘Kaizen’ event can be implemented to mark improvement. The first step of Kaizen implementation commences with a message from the leadership, detailing what is going to happen and why it is important.31 This directive also gives the improvement team a go-ahead to implement the changes and carefully document the outcomes. By the end of day, the team should be fully aware of what they will be doing over the next several days.10 The second step starts with a review of the course of action. The team identifies problematic areas, then brainstorms methods to address the identified problems. The day ends with a report to leadership. The third step begins with implementation, where the team is divided into smaller, tasked groups. Communication among the teams should be transparent so that everyone knows the progress made. The fourth step is the implementation of the process tested the day before. Each team member takes up a role, and when it is finally tried, healthcare providers should see the effect of the new process in the outcomes.10
The trial should run for eight hours at most, with keen observation, If the outcome is positive, then the emergency department proceeds or improvements are added. This happens in a wrap-up discussion at the end of day four. Finally, in the fifth step, the team presents to the leadership. The team then creates a future action plan to maintain the improvements. Within approximately one week, healthcare providers who come together can improve flow and remove waste. Consequently, measures should be in place to minimize resistance, such as effective communication and transparency as to why changes are taking place.
Prolonged Boarding and Slow Diagnosis
Diagnosis is the most important stage in the management and treatment of any patient, as through this process health providers are able to identify the problem and provide effective patient-centered care. In emergency, triage accuracy is affected by the nurse’s training related to mental health problems.32,33 It is hard to diagnose a mental issue in comparison to a physical one, which can cause delays in treatment.34 Slow diagnostic processes in emergency departments have been attributed to several causes including delayed psychiatric boarding, ineffective communication, lack of human resources and mandatory medical clearances.11
Delayed psychiatric boarding, defined as patients’ waiting in hallways or other areas for inpatient beds is a major problem.11 Mental health patients have a significantly greater length of stay in the emergency department compared to those with physical illness.35 Prolonged psychiatric boarding has multiple causes, including a shortage of inpatient beds, limited access to mental health clinicians, insufficient community mental health services and an increased number of patients with drug abuse.11 Staff attitudes may also prolong the process, whereby providers pay greater attention to patients suffering from other conditions.11 The long diagnostic process is caused by lack of collaboration and effective communication among physicians, staff and patients where the majority may not be mentally capable of communicating.10,36 This communication is important to ensure that providers have real-time insights, information, medical history and data that are required to swiftly make a diagnosis and understand the treatment needs of the patient. Effective communication between patient and staff is also important to improve the triage process.8 A third factor leading to delayed diagnosis is lack of human resources or trained staff.10 Fourth, medical clearance is used to identify whether a medical illness is contributing to mental health issues.37 This can slow the process, but the SMART medical clearance process avoids lengthy testing procedures when unnecessary.
Tucci et al., recommend that all emergency physicians should have a basic understanding of the diagnosis and treatment of psychiatric emergencies.38 In addition, they should have a grasp of the legal regime that guides treatment in their jurisdiction. Boarding, poor collaboration and communication among caregivers who handle mental health patients in the emergency department also contribute to the sluggish flow. This problem can be solved by incorporating treatment teams including emergency physicians and psychiatrists.10 Maintaining the flow of patients can produce the best results using a dedicated separate psychiatric unit within the emergency department. Such a unit can provide privacy, decrease waiting time and enhance patient care because they have the capability of handling mental health patients effectively.10
Many emergency departments have tried assigning crisis workers to help physicians before referring them to psychiatric services, but the complexity and similarities between the signs and symptoms of mental health issues also plays a significant role in the diagnostic process.39 The majority of mental health issues are diagnosed using the symptoms that patients exhibit at the time of admission, and many present overlapping symptoms. Diagnosis takes time and specialized training. As a result, more psychiatrists are being recruited.40
Emergency departments can reduce boarding time through telepsychiatry, observation, evaluation, treatment, re-evaluation zones, and mobile crisis units, within the emergency department.41 Psychiatric observation units in the emergency department help with boarding. A psychiatrist in the emergency department can reduce the time it takes for assessment and diagnosis. A second advantage of the separate psychiatric unit is that mental health patients do not have to compete for attention with other patients.
Similarly, Zeller proposes the emPATH (emergency Psychiatric Assessment, Treatment & Healing unit) model. The model is executed by safely and effectively diagnosing, treating and boarding patients, leading to fewer hospitalizations.39 In addition, emPATH units allow for moving individuals in crisis into separate care, which opens up emergency department beds and is more cost-effective.39
Interventions to Improve and Maintain Patient Safety
Providing mental healthcare in a high-quality manner is pivotal to the safety of patients, and healthcare providers.42 Roughly half of mental healthcare providers have been physically assaulted by patients, which puts these workers at higher risk of violence than other staff. Unfortunately, the design of most emergency departments poses safety concerns.43 One study showed that 37% of emergency department rooms do not have doors lockable from the inside or two-way doors 35% had furniture and equipment likely to cause harm, and 25% of the rooms had only one door.43 One of the most important measures that hospitals can take is to develop better training programs aimed at preventing workplace violence. A critical component of training is de-escalation.
The first measure is to move agitated patients away from public spaces into secure rooms.30 Second, the space should be devoid of items likely to escalate the patient’s condition, or with which the patient might use as a weapon44 Other measures include implementing environmental controls (minimizing lighting and noise). Bolton et al., described the safety criteria that should be available: assessment rooms should be located within the main emergency department and should have two doors, an observation panel, a panic button or alarm system, and only include items unlikely to be used to cause harm.43
Concerns have emerged that some healthcare professionals use restraints unnecessarily.45 According to the College of Nurses of Ontario restraints should be used only after an accurate assessment of the mental state of an individual.46 While restraints should be temporary, some providers place patients in restraints for lengthy periods of time, which may extend the patient’s already prolonged stay.10 These practices create feelings of helplessness, humiliation, and shame and can dissuade patients from seeking help in the future.47 In addition, providers are perceived to routinely apply chemical restraints, designed to sedate.48 This leads to admitting the patient for continuous observation even when not needed which uses greater resources.48 Healthcare workers should allow patients to regain self-control and avoid physical restriction since this typically strengthens the belief that violence represents the most fitting solution.49
Patients should be involved in their care plan. For instance, the caregiver can offer the patient choices that determine how their interaction unfolds and should treat the patient with respect, speak calmly and enable personal space.50 Meanwhile, the treatment team should be on standby in order to step in promptly if needed.10 However, all staff who handle mental health patients should be trained in dealing with safety risks.42
Stowell et al., and Dzubak summarize key risk areas that can increase safety when handling mental health patients including; training, awareness, environmental safety, boundaries, control, and knowing oneself.49,50 The training equips caregivers with crisis intervention skills and safe de-escalation techniques. Awareness, on the other hand, ensures that the staff knows how to use safety resources as required.51 Environmental safety ensures that mental health patients cannot find anything to use as a weapon.50 Caregivers must establish firm limits with mental health patient so that they do not abuse boundaries. Caregivers should monitor their feelings and emotions.51
Improving Health Care Workers' Knowledge, Competency, and Attitudes
Emergency department providers are required to complete continuing education however, poorly trained staff are one of the obstacles to comprehensive care.22 Most providers pay greater attention to patients they are confident serving.51 Emergency department staff attributed their discomfort to a feeling of inadequacy, which stems from lack of training.22
In cases where a dedicated psychiatric unit in the emergency department is not feasible, Balan, calls for an adjustment to the training curriculum.10 Lack of consistency and limited mental health education courses contribute to the lack of preparedness of emergency department nurses.1 Necessary skills should include the ability to triage, assess and accurately diagnose mental health patients promptly and provide the required comprehensive care. The psychiatric emergency service approach requires these patients be admitted to the psychiatric unit as soon as possible or discharge them home with a proper plan of care within 24 hours, and to safely continue treatment in a community health centre.27
Improving the Discharge Planning and Follow up Process
In Canada, access to mental health services is a concern. A 2011 Ontario study showed that more than half of newly diagnosed mental health patients did not see a specialist within 30 days of referral.52 Access to specialty psychiatric care may decrease the deterioration of problems and minimize subsequent visits to already overcrowded emergency departments.53 Emergency departments have difficulty with post discharge instructions.54 Working pressure, the nature of the busy environment, and conflicts in the emergency department are barriers associated with ineffective discharge.54 Instructions for follow-up appointments are not consistently clear. Moreover, the discharge plan may be incomplete, and patient understanding of post-discharge care is below standard.55 Engel et al., found that 39% of patients did not understand their discharge instructions; increased focus on follow-up may help patients maintain treatment and reduce return visits.54
Another negative impact of a poor follow-up process is preventing emergency healthcare workers from identifying misdiagnoses. Follow-up can provide an opportunity to determine whether the condition has been correctly diagnosed and treated. Once again, the perception of mental health issues as less serious may partly explain why healthcare workers do not pay more attention to the follow-up care of psychiatric patients. Regardless, the shortcomings of the existing strategies have resulted in the development of a “revolving door” whereby mental health patients leave the emergency department only to come back later in a seemingly never-ending cycle.23 Further, poor follow-up strategies leave many patients with poor-quality treatment which affects the management of further complications.56 Poor follow-up prevents providers from determining whether patients are complying with their therapeutic plans. Patients experiencing homelessness for example, typically return and experience frequent hospitalization because of social and economic factors.
Outpatient follow-up is an important indicator of the quality of healthcare at hospitals. Pfeiffer et al., found that earlier follow up for mental health patients might be effective at engaging them in care, and decreasing the chance of return visits and readmissions.57 A growing number of emergency departments have started to implement strategies to ensure mental health patients receive the necessary care and proper follow up.53 One of these strategies is to set up an effective discharge planning system including follow-up appointments, discharge instructions and sending a written referral letter to an outpatient specialty clinic.55 Management of transitions from inpatient to outpatient services is a key element of effective continuity of care. The Guided Care Model focuses on training a special nurse who works in primary care and communicates with patients and their family educating and empowering them. They also work with community agencies to ensure the patient receives the appropriate community, social and mental support for their needs.
Another option to improve follow-up care is the Trieste model.20 The Trieste Department of Mental Health has four community mental health centers that operate 24 hours every day, alongside a general hospital psychiatric unit and housing facilities, with social and work enterprises.19 Together, these provide for a complete and effective path to recovery. The Trieste system is seamlessly integrated such that whenever a patient is registered, they have the necessary care and continuous follow up service until fully recovered.58 The system has the capacity to accommodate chronic cases on a long-term basis. To be able to manage new, ongoing, and chronic cases effectively, healthcare providers from different specialties have defined roles.20 Every feature of this system epitomizes a complete follow-up, because the system goes as far as providing social and economic support to the family members of mental health patients to enable recovery.19 For this system to include the provision of care for family members means that it captures most details that may have relevance to the condition of patients.
In Canada59 community mental health services need to be better funded to provide early assessment and prevention, enhanced mental healthcare and treatment and longer-term follow-up and supervision for those with severe mental health problems. Moreover, the mental health system has to address the challenges associated with follow-up after discharge, and they must invest significantly in developing community-based support structures. In addition, emergency departments require a dedicated psychiatric zone, to conduct the necessary follow-up for patients in crisis. Moreover, these dedicated units would be in a position to build a closer working relationship with community-based mental health resource networks to ensure that patients receive temporary accommodation or other support if needed.58 Furthermore, while this is costly, this investment can be viewed as part of a larger scheme that seeks to improve mental healthcare delivery. It is apparent that this sector of healthcare has been underfunded for many years; however, there is no shortcut to improving mental healthcare other than investing in it.60
Summary
Improved diagnostic and boarding processes can be accomplished through a psychiatric observation unit; the emPATH model is effective, as is the use of treatment teams and partnering physicians with psychiatrists.39 Use of SMART medical clearance can speed up assessment. Improved patient safety de-escalation strategies reduce risk.43 Patients should be involved in their care plan and given some sense of control. Respectful treatment of patients is important.30
Improvement in healthcare workers’ knowledge, competency and attitudes toward mental health patients is crucial.10 Proper discharge planning includes the use of follow-up appointments, clear discharge instructions, and referrals to outpatient clinics. The Trieste model that supports mental health patients during and after their return to the community is an ideal to strive for.20 The capacity of both inpatient and community mental health services needs improvement. Telemedicine could be increased, and the employment of Lean management is becoming popular.25
Guidelines on Providing Optimal Mental Health Care in the Emergency Department
Emergency departments will continue to receive mental health patients because they are the only place to go.23 Until there are robust community-based resources, emergency departments have to provide the best care possible. Appropriate staffing is key.10 When mental health patients walk through the emergency department doors, whether accompanied by family or not, there should be staff that direct them to triage. The time between intake and boarding should be minimized. Many studies have found that using physicians, along with triage, improves door-to-provider time, patient satisfaction, and decreases the percentage of “left-without-being-seen” patients.61
To improve patient flow, low acuity patients should be directed to community-based services, to allow specialized emergency physicians to deal with high priority patients.60 These patients should undergo medical clearance quickly.37 Then, the physician refers the patient to a psychiatrist for a comprehensive evaluation. The outcome of this assessment determines whether a patient is discharged or admitted. For low acuity patients, the psychiatrist should develop a treatment plan and then hand the patient over to the discharge team. For those requiring further observation, the psychiatrist can develop a treatment plan to be provided by a multidisciplinary team to help improve outcomes and increase patient and employee satisfaction.10
To decrease pressure on emergency departments, the boarding process should be quick. An Australian study suggested a flow model that improved the average time to admission to four hours from eight hours.34 The length of stay in the emergency department was reduced by 41 minutes. This flow depends on the “Pull from the emergency department service delivery model” which refers to the concept of patient flow; hospital floor providers ask for emergency patients, by going down to emergency to pull their admitted mental health patients rather than the emergency healthcare providers bringing (pushing) the patients upstairs to the psychiatric floor.
Studies have shown that improvements in hospital discharge planning can enhance outcomes for patients.56 In addition, timely outpatient mental health follow-up results in benefits for both the patient and the healthcare system, including increased rates of recovery, decreased readmissions and decreased pressure on the emergency department; resulting in improved quality of care.57 The patient should be provided with the names of the psychiatric ward, attending physicians and the primary nurse, as well as an expected date of discharge from the hospital and appropriate referral to a community centre for the continuation of the treatment plan as an outpatient.10
Conclusion
Emergency departments are seeing an increasing number of visits by mental health patients but they are not equipped to take over comprehensive care.6 Emergency departments are available around the clock but, poorly designed as the environment is cold, noisy and disliked. They have long wait times and limited access to food, drink and other necessities. Mental health patients generally feel dissatisfied after their visits.1,2 Although mental health patients are one of the most vulnerable groups to visit emergency departments, they often receive suboptimal care and treatment.10,62
Many problems are systems-based and thus require systems-based solutions. These barriers include a reduction in psychiatric beds; a lack of resources, especially during busy hours; delayed and long diagnostic processes; safety concerns: suboptimal training of staff; and poor follow-up. Moreover, in many emergency departments, comprehensive care of mental health patients continues to follow the model of acute physical illness.62 Addressing this situation requires improved educational opportunities and funding, specifically for the improvement of community healthcare systems.63
To ensure mental health patients receive appropriate, quality care, increased effort is required to overcome obstacles and barriers that prevent healthcare workers in the emergency department from providing comprehensive care. Solutions are suggested for each barrier, including improved resources and inpatient psychiatric beds, emergency department redesign, and improved linkage with community resources.39,63 At the same time, it is important to develop connections between community-based outpatient, crisis, inpatient, and emergency department services.
The need for more educational opportunities in mental health for the emergency department staff is imperative.1 In addition, to achieve improvements in providing comprehensive care to mental health patients, the Lean system was identified as one of the most effective models as it allows for solving emergent problems in real time.29 Most importantly, it focuses on continuous improvement, which is pivotal to success. This makes it a good fit for enhancing treatment outcomes for patients experiencing a mental health crisis.29 Another way to improve healthcare is to use tele-psychiatry.64
Improvements require funding. Some redesign of emergency departments is occurring and there is a definite trend toward more effective community-based care for mental health patients. More training of a practical nature is also being offered to emergency department staff. These are encouraging signs. Implementation of separate emergency departments for mental health patients and more strategic planning for discharge and follow up are recommended and more attention should be paid to the medical clearance of mental health patients. With attention to the recommendations made in this paper concrete progress can be achieved in the comprehensive care needed by mental health patients in emergency departments.
Conflict of Interest
The authors have no conflicts of interest to declare.
References
- Innes K, et al. Caring for the mental illness patient in emergency departments-an exploration of the issues from a healthcare provider perspective. Journal of Clinical Nursing. 2014; 23(13-14): 2003-2011.
- Clarke D, et al. Emergency department staff attitudes towards mental health consumers: A literature review and thematic content analysis. International Journal of Mental Health Nursing. 2014; 23(3): 273-284.
- Zun L, Downey L. Identifying Undiagnosed Pediatric Mental Illness in the Emergency Department. Annals of Emergency Medicine. 2012; 60(4): S99.
- Khan S, et al. Use of Mental Health Services by Youths and Young Adults Before and During Correctional Custody: A Population-Based Study. Psychiatric Services. 2016; 67(7): 790-793.
- Canadian Institute for Health Information (CIHI) [Internet]. Child and youth mental health in Canada – Infographic; 2017, June 08. Available from: https://www.cihi.ca/en/child-and-youth-mental-health-in-canada-infographic
- Gill PJ, et al. Emergency department as a first contact for mental health problems in children and youth. Journal of the American Academy of Child & Adolescent Psychiatry. 2017; 56(6): 475-482.
- Wohlford-Neubauer S. The Lived Experiences of Emergency Department Personnel in Working with Individuals with Mental Health Needs. 2016.
- Broadbent M, Moxham Land Dwyer T. Implications of the emergency department triage environment on triage practice for clients with a mental illness at triage in an Australian context. Australasian Emergency Nursing Journal. 2014; 17(1): 23-29.
- Harris B, et al. Patients’ experiences of psychiatric care in emergency departments: A secondary analysis. International Emergency Nursing. 2016; 26: 14-19.
- Balan Y, Murrell K, Lentz CB. Big Book of Emergency Department Psychiatry: A Guide to Patient Centered Operational Improvement. United Kingdom: Routledge.
- Alakeson V, Pande N, Ludwig M. A plan to reduce emergency room ‘boarding’ of psychiatric patients. Health Affairs. 2010; 29(9): 1637-1642.
- Niles C. Examining the deinstitutionalization movement in North America. Health Tomorrow: Interdisciplinarity and Internationality. 2013; 1(1).
- Dyck E. Dismantling the asylum and charting new pathways into the community: Mental health care in twentieth century Canada. Histoire sociale/Social history. 2011; 44(2): 181-196.
- Scheid TL, Wright ER. A handbook for the study of mental health. United Kingdom: Cambridge University Press. 2017.
- Novella EJ. Mental health care in the aftermath of deinstitutionalization: a retrospective and prospective view. Health Care Analysis. 2010; 18(3): 222-238.
- Primeau A, et al. Deinstitutionalization of the mentally ill: Evidence for transinstitutionalization from psychiatric hospitals to penal institutions. Comprehensive Psychology. 2013; 2(1).
- Shen GC, Snowden LR. Institutionalization of deinstitutionalization: a cross-national analysis of mental health system reform. International Journal of Mental Health Systems. 2014; 8(1): 47.
- Chang G, et al. Hospital variability in emergency department length of stay for adult patients receiving psychiatric consultation: a prospective study. Annals of emergency medicine. 2011; 58(2): 127-136.
- Frances AJ. World's best and worst places to be mentally ill. Psychology Today; 2015. Available from: https://www.psychologytoday.com/us/blog/saving-normal/201512/worlds-best-and-worst-places-be-mentally-ill
- Portacolone E, et al. A tale of two cities: The exploration of the Trieste public psychiatry model in San Francisco. Culture, Medicine, and Psychiatry. 2015; 39(4): 680-697.
- Yohanna D. Deinstitutionalization of people with mental illness: causes and consequences. AMA Journal of Ethics. 2013; 15(10): 886-891.
- Zun L. Care of psychiatric patients: the challenge to emergency physicians. Western Journal of Emergency Medicine. 2016; 17(2): 173.
- Wise-HarrisD, et al. “Hospital was the only option”: experiences of frequent emergency department users in mental health. Administration and Policy in Mental Health and Mental Health Services Research. 2017; 44(3): 405-412.
- Jung C. Thunder Bay hospital plans to redesign emergency department for mental health patients, seeks funding. CBC News. 2018. Available from: https://www.cbc.ca/news/canada/thunder-bay/thunder-bay-emergency-redesign-1.4739819
- Francisco K, Archer NP. The impact of telemedicine on primary mental health care in Canada. 2015.
- Southland E, Neufeld J, Laws S. Telemental health evaluations enhance access and efficiency in a critical access hospital emergency department. Telemed J E-Health. 2014; 20: 664-668.
- Zeller S. Dedicated psychiatric emergency services reduce the need for inpatient hospitalizations. Vituity. 2018. Available from: https://www.vituity.com/blog/dedicated-psychiatric-emergency-services-reduce-the-need-for-inpatient-hospitalizations
- Rutman L, et al. Improving patient flow using lean methodology: an emergency medicine experience. Current Treatment Options in Pediatrics. 2015; 1(4): 359-371.
- Balfour ME, et al. Using lean to rapidly and sustainably transform a behavioral health crisis program: Impact on throughput and safety. The Joint Commission Journal on Quality and Patient Safety. 2017; 43(6): 275-283.
- Weiland TJ, et al., Optimal management of mental health patients in Australian emergency departments: barriers and solutions. Emergency Medicine Australasia. 2011; 23(6): 677-688.
- Holden RJ. Lean thinking in emergency departments: a critical review. Annals of emergency medicine. 2011; 57(3): 265-278.
- Bullard MJ, et al. Revisions to the Canadian emergency department triage and acuity scale (CTAS) guidelines. Canadian Journal of Emergency Medicine. 2014; 16(6): 485-489.
- Clarke D, et al. How will you triage this mental health presentation: it depends. In International Emergency Nursing. 2014; 22(4): 274.
- Bost N, et al. Clinician perspectives of a mental health consumer flow strategy in an emergency department. Collegian. 2018; 25(4): 415-420.
- Affleck A, et al. Emergency department overcrowding and access block. Canadian Journal of Emergency Medicine. 2013; 15(6): 359-370.
- Kubiel TJ. Transforming Care of the Behavioral Health Patient in an Emergency Department Setting. 2016.
- Anderson EL, et al. American Association for Emergency Psychiatry Task Force on Medical Clearance of Adults part I: introduction, review and evidence-based guidelines. Western Journal of Emergency Medicine. 2017; 18(2): 235.
- Tucci V, et al. Down the rabbit hole: emergency department medical clearance of patients with psychiatric or behavioral emergencies. Emergency Medicine Clinics. 2015; 33(4): 721-737.
- Zeller S. EmPATH units as a solution for ED psychiatric patient boarding. Psychiatry Advisor; 2017. Available from: https://www.psychiatryadvisor.com/home/practice-management/empath-units-as-a-solution-for-ed-psychiatric-patient-boarding/
- Goldner EM, Bilsker D, Jenjins E. A concise introduction to mental health in Canada. Toronto: Canadian Scholars’ Press. 2016.
- Brown MD, et al. Clinical policy: critical issues in the diagnosis and management of the adult psychiatric patient in the emergency department. Annals of Emergency Medicine. 2017; 69(4): 480-498.
- Kelly EL, et al. Well-being and safety among inpatient psychiatric staff: the impact of conflict, assault, and stress reactivity. Administration and Policy in Mental Health and Mental Health Services Research. 2016; 43(5): 703-716.
- Bolton J, Palmer L, Cawdron R. Survey of psychiatric assessment rooms in UK emergency departments. BJPsych bulletin. 2016; 40(2): 64-67.
- Plant LD, White JH. Emergency room psychiatric services: a qualitative study of nurses’ experiences. Issues in Mental Health Nursing. 2013; 34(4): 240-248.
- Brophy LM, et al. Consumers and their supporters’ perspectives on poor practice and the use of seclusion and restraint in mental health settings: results from Australian focus groups. International journal of mental health systems. 2016; 10(1): 6.
- Adam S. Crazy making: the institutional relations of undergraduate nursing in the reproduction of biomedical psychiatry. International journal of nursing education scholarship. 2017; 14(1).
- Pearl FR. Improving patient safety by decreasing restraint use (Master’s Thesis). The University of San Francisco, California, United States. 2015.
- Hu F, et al. An examination of the incidence and nature of chemical restraint on adult acute psychiatric inpatient units in Adelaide, South Australia. International journal of mental health nursing. 2019.
- StowellKR, et al. Psychiatric Evaluation of the Agitated Patient: Consensus Statement of the American Association for Emergency Psychiatry Project BETA Psychiatric Evaluation Workgroup. Western Journal of Emergency Medicine. 2012; 13(1): 11-16.
- Dzubak JL. Managing mental health emergencies in the ED: Safety and continuity are key to successful care. American Nurse Today. 2017; 12(11). Available from: https://www.americannursetoday.com/managing-mental-health-emergencies-ed/
- Giandinoto JA, Edward KL. Challenges in acute care of people with co-morbid mental illness. British Journal of Nursing. 2014; 23(13): 728-732.
- RudolerD, et al. Payment incentives for community-based psychiatric care in Ontario, Canada. CMAJ. 2017; 189(49): E1509-E1516.
- Kurdyak P, et al. Impact of physician follow-up care on psychiatric readmission rates in a population-based sample of patients with schizophrenia. Psychiatric Services. 2017; 69(1): 61-68.
- Engel KG, et al. Patient understanding of emergency department discharge instructions: where are knowledge deficits greatest? Academic Emergency Medicine. 2012; 19(9): E1035-E1044.
- Horwitz LI, et al. Quality of discharge practices and patient understanding at an academic medical center. JAMA internal medicine. 2013; 173(18): 1715-1722.
- Carson NJ, Vesper A, Chen CN, et al. Quality of follow-up after hospitalization for mental illness among patients from racial-ethnic minority groups. Psychiatric Services. 2014; 65(7): 888-896.
- Pfeiffer PN, et al. Outpatient follow-up after psychiatric hospitalization for depression and later readmission and treatment adequacy. Psychiatric Services. 2012; 63(12): 1239-1242.
- Mezzina R. Community mental health care in Trieste and beyond: An “Open Door–No Restraint” system of care for recovery and citizenship. The Journal of nervous and mental disease. 2014; 202(6): 440-445.
- Canadian Mental Health Association. Mental health in the balance: Ending the health care disparity in Canada. Canadian Mental Health Association. 2018.
- Lake J, Turner MS. Urgent Need for Improved Mental Health Care and a More Collaborative Model of Care. The Permanente Journal. 2017.
- Weston V, et al. Effectiveness of resident physicians as triage liaison providers in an academic emergency department. Western Journal of Emergency Medicine. 2017; 18(4): 577.
- Tyerman JJ. Registered nurses’ experiences of care for individuals with mental health issues in the emergency department (Master’s thesis). Queen’s University, Kingston, Ontario, Canada. 2014.
- Cohen KR, Peachy D. Access to psychological services for Canadians: Getting what works to work for Canada’s mental and behavioural health. Canadian Psychology/Psychologie Canadienne. 2014; 55(2): 126.
- Narasimhan M, et al. Impact of a telepsychiatry program at emergency departments statewide on the quality, utilization, and costs of mental health services. Psychiatric Services. 2015; 66(11): 1167-1172.
